#FullRepeal Daily Digest
Heritage Foundation: New Obamacare Enrollment Data: Employer-Based Coverage Declines
- New data show that the number of people who have private health insurance increased by just over 520,000 in the six months between October 1, 2013, and March 31, 2014. That was because almost all the gains in individual coverage through the Obamacare exchanges were offset by reduced enrollment in employer-sponsored group coverage.
- During the same period, Medicaid enrollment increased by about 5 million, principally as a result of Obamacare expanding eligibility to able-bodied adults without dependent children. Because of delays in the exchanges processing enrollments and a “surge” in exchange applications in March, it is possible that a further 3 million to 4 million individuals may have gained individual coverage since March 1. However, even if that proves to be the case, and even if there is no further erosion in employer coverage, more than half of any increase in coverage during 2014 will still be due to Obamacare’s expansion of Medicaid.
Forbes: A Hippocratic Tragedy
- At the end of 2014, the Centers for Medicaid and Medicare Services will start penalizing doctors, hospitals, and other health care providers for not participating in the Physician Quality Reporting System. Originally introduced in 2007 as a voluntary program, PQRS asks providers to report on their compliance with pre-approved treatment paradigms for their Medicare patients. Doctors must obtain various health data on at least 80 percent of patients, which they must then submit to CMS. Until 2014, providers who met this goal received a monetary bonus.
- This is a dagger aimed at the heart of medicine—it can perversely encourage doctors to limit the number of patients with complex medical problems they see. Why? Because those patients may need treatments that fall outside the program’s cookie-cutter protocols or they may require lengthy and frequent attention. This may jeopardize a doctor’s ability to meet the PQRS quota. Potentially affected patients may have conditions including diabetes, cardiovascular disease, etc., all which can make the management of a patient’s other medical conditions more difficult to treat.
- Enter Obamacare. It forces the majority of doctors to join PQRS by levying a penalty on non-participating doctors. (It also eliminates the bonus). The penalty starts in 2015 at a 1.5 percent cut on a doctor’s Medicare reimbursement rate, rising to a 2 percent cut in 2016 and beyond. While the program is still technically voluntary, Medicare’s low reimbursement rates give most doctors little choice but to give in to this financial coercion.
- Every doctor who works at a hospital or anything but a private practice—a percentage that increases by the year—will have no choice but to participate in PQRS reporting. The only way to avoid it will be to refuse to accept Medicare—something that a growing number of doctors, including myself, have done.
- [in another instance]…CMS recently began assessing a penalty for hospitals that readmit too many Medicare patients within 30 days of their initial treatment. While the reasoning behind this is straightforward enough—doctors must not be doing their job if their patients frequently return with the same problems—it fundamentally misunderstands that every patient has unique medical needs. This simple truth means that some patients may require more frequent treatment, particularly if they have a recurring or rare medical issue.
- Yet absent any nuance, the CMS rule leaves doctors with a financial reason not to see the patients who need help the most. In the future, patients with diabetes, high blood pressure, heart disease, and other serious medical issues may find it increasingly difficult to find doctors willing to take care of them.
- It’s a similar story with Obamacare’s January 2014 revamp of the Evaluation and Management Coding system, the billing process used for Medicare patients. Prior to the law, E&M utilized five different codes for hospital clinic visits, which scaled reimbursement rates based on complexity.
- In January, CMS replaced the five-code system with a single code and a single reimbursement rate for all hospital-employed physicians. In my field, for instance, a doctor who spends a few minutes getting wax out of someone’s ear gets paid the same as a doctor spending an hour evaluating, planning surgery and counseling a patient with an extensive skull base tumor.
- This is little different than the changes to PQRS. It incentivizes doctors—and the hospitals that employ them—to prioritize quick and simple patient visits over long and complex procedures. As elsewhere, the government is placing financial incentives over patient well-being. This, again, punishes doctors that take care of patients who need medical care the most.
Forbes (John Goodman): Medicare Hype
- The latest Medicare Trustees report was released yesterday and there were two main messages in the administration’s press release: (1) slower Medicare growth has added four more years to the life of the Medicare Trust Fund, relative to last year’s report, and (2) the main reason is the Affordable Care Act (ObamaCare), including new payment methods the administration has been experimenting with and the establishment of Accountable Care Organizations (ACOs).
- If a private pension fund made claims like this the Justice Department would probably have the guilty parties up on charges of fraud...the Medicare Trust Fund holds no real assets. All Medicare taxes and premium payments go to the Treasury and all that money has already been spent. All the Trust Fund represents is a giant IOU the federal government has written to itself. Medicare, in other words is run like a Bernie Madoff scheme. That’s why it has a huge unfunded liability totaling trillions of dollars.
- Devon Herrick explains:
- “The Trustees Report is supposed to project future Medicare spending based on current law. But, that also means the official projection includes provisions meant to slow spending growth that the Trustees know are unlikely to occur. In years past, the Trustees tended to ignore these uncomfortable facts. Around 2010 the Office of the Actuary at CMS took the unprecedented step of producing an Alternative Scenario report explaining that the assumptions in the Trustees Report were unrealistic, and the projection were most assuredly wrong. That raised eyebrows in the policy world. This year, the alternative scenarios (i.e. conditions that are more likely to occur) crept up from the appendix (at the back) and landed uncomfortably on page 2.”
- ”Current law requires CMS to implement a reduction in Medicare payment rates for physician services of almost 21 percent in April 2015. However, it is a virtual certainty that lawmakers will override this reduction as they have every year beginning with 2003.”
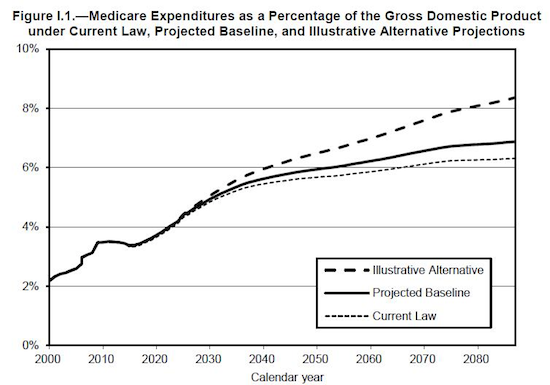
- [in the chart above] the upper most line (the path the Trustees consider most likely and which is completely ignored in the HHS press release) is 50% higher than current law spending because once again, current law makes unrealistic assumptions about other Medicare spending cuts.
- What exactly is “current law”? It’s ObamaCare. When President Obama signed the Affordable Care Act he wiped out about $52 trillion in Medicare’s unfunded liability? How did that happen? He did it with pen and ink. For the first time ever, federal law has imposed a global cap on total Medicare spending and this cap is to be enforced regardless of the medical needs of the elderly!
![]()
